Endoscopy (Colonoscopy & Gastroscopy)
The endoscopy procedure uses an endoscope to examine the interior of a hollow organ or cavity of the body for disease.
The endoscopy procedure uses an endoscope to examine the interior of a hollow organ or cavity of the body for disease.
What is Endoscopy (Endoscopic surgery)?
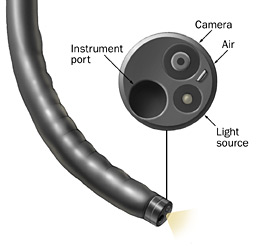
Endoscopic surgery is a minimally invasive procedure aiming at examining the lumen of the digestive tract using an endoscope, which is a flexible tube with a light and a camera attached to it. That way, the surgeon is able to view the imaging on a flat colour TV screen. Each endoscope contains an instrument port, through which specially designed devices can be safely introduced for specific actions; for instance biopsy forceps, snare for polyp removal, or endoscopic basket for extraction of foreign body.
Gastroscopy (Upper Endoscopy)
Gastroscopy or Upper GI Endoscopy is usually indicated for patients with symptoms of the upper gastrointestinal tract that may include, abdominal pain, bloating, reflux symptoms, vomiting, or bleeding. While the patient is under sedation, an endoscope is introduced through the mouth and gradually advanced down the oesophagous, stomach and part of the small bowel (duodenum). If required, biopsies may be performed and pictures taken. The most common pathologies identified are: hiatus hernia, peptic ulcer, Helicobacter pylori infection, lactose intolerance, or gluten intolerance.
Gastroscopy is very safe and patients normally go home on the same day of the procedure. They should avoid driving for the next 24 hours following their endoscopy.
Flexible sigmoidoscopy is generally indicated when looking for a cause of bright red bleeding of the lower gastrointestinal tract, generally following bowel motions in the toilet bowl or on toilet paper. The scope is inserted through the rectum, allowing detailed examination of the distal part of the large bowel. The most common causes of lower gastrointestinal bleeding include internal haemorrhoids, bowel inflammation (ulcerative colitis), diverticular disease or benign arteriovenous malformation (angiodysplasia).
This endoscopic surgery requires a pre-operative enema to clean the lower part of the colon and rectum. Flexible sigmoidoscopy is done under sedation, is brief, safe, and does not cause much discomfort besides abdominal bloating (wind pain) that usually rapidly settles. Patients normally go home on the same day and should avoid driving for the next 24 hours following their endoscopy.
At the end of a flexible sigmoidoscopy, if no other source of bleeding has been found it is very quick and easy to perform a simple rubber band ligation of internal haemorrhoids. Rubber bands (generally 2 or 3) are placed at the base of each enlarged internal haemorrhoids to constrict the blood supply, causing them to become ischaemic (dead tissue) and spontaneously fall off from the bowel wall after 3 to 10 days. This treatment is rarely painful and passing the detached haemorrhoids with the bowel movements remains generally unnoticed by the patients. On very few occasions significant fresh blood per rectum may occur after haemorrhoids fall off, but this generally subsides under conservative management.
Colonoscopy is quite similar to a flexible sigmoidoscopy. The only difference is that the colonoscope is gradually advanced throughout the entire length of the colon where the appendix is attached to, or even further into the most distal part of the small bowel (terminal ileum) when necessary. Most common indications for colonoscopy include iron deficiency anaemia, dark stools, positive faecal occult blood test (FOBT), change of bowel habit, surveillance after colonic polypectomy or cancer resection, and past family history of bowel cancer.
A bowel preparation is mandatory in order to obtain and excellent view of the mucosa (lining of the rectum, colon and small bowel). This bowel cleansing is started 24 hours prior to the procedure and patients should remain on clear fluids from that time until around three hours before endoscopy. Colonoscopy is done under sedation, takes around 30 minutes to be completed and does not cause much discomfort besides abdominal bloating (wind pain) that rapidly settles while recovering from the procedure. Patients normally go home on the same day and should avoid driving for the next 24 hours following their endoscopy.
Although very safe, the major risk associated with colonoscopy is bowel perforation that may occur in one in every 800 to 1,000 procedures. If this was to happen, conservative management with bowel rest and intravenous antibiotics is the first line of treatment. Sometimes, a laparoscopic (keyhole) exploration is necessary for closure of the bowel defect. Very rarely, large bowel resection with temporary diverting colostomy (Hartmann’s procedure) may be necessary to treat the complication. This is generally reversed within few months.
If you would like to book an appointment for a consultation or procedure please call us or use our online booking form