Acid reflux is the result of stomach acid (often combined with bile) refluxing back into the oesophagous and typically causing a sensation known as “heartburn” (lower to mid-chest pain, burping and food regurgitation). Sometimes, patients may also complain of change of voice, swallowing or breathing difficulty, nausea, sore throat, night-time coughing or recurrent chest infection.
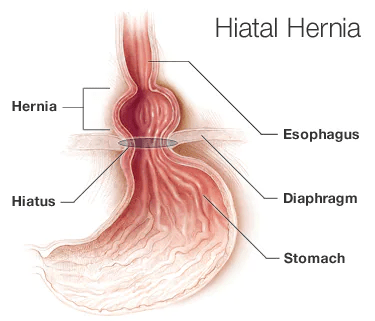
This disorder is also called gastro-oesophageal reflux disease (GORD) and is caused by a weakness of the circular lower oesophageal sphincter (LOS). The LOS is normally situated below the diaphragm and acts like a valve preventing stomach content from moving back into the oesophagus. When a hiatus hernia (HH) is present, the LOS is progressively displaced upwards into the chest, as the stomach bulges through a hole in the diaphragm. With time the HH increases in size thus exacerbating reflux symptoms, as the LOS becomes unable to fulfill its role as an anti-reflux flap valve mechanism. Additionally, certain factors such as obesity, pregnancy, smoking, alcohol, or food (chocolate, garlic, caffeine, spicy food, citrus) may impair even further its function thus aggravating GORD.